The State Of Mental Healthcare: Challenges And Opportunities For Improvement

Table of Contents
Access to Mental Healthcare: A Persistent Barrier
Access to mental healthcare is a fundamental right, yet millions worldwide struggle to receive the care they need. Several key factors contribute to this persistent barrier:
-
Geographic disparities: The unequal distribution of mental health professionals creates significant challenges, particularly in rural and underserved communities. Individuals in these areas often face long travel times to appointments, lack of transportation options, and limited access to specialized care. This disparity directly impacts mental health access and outcomes.
-
Financial barriers: The high cost of mental healthcare, including therapy, medication, and hospitalization, poses a significant obstacle for many. Limited insurance coverage, high deductibles, and co-pays can make treatment unaffordable, forcing individuals to forgo necessary care or delay seeking help. This financial burden disproportionately affects low-income individuals and families.
-
Long wait times: Delays in accessing appointments and treatment are a widespread problem, often leading to worsening conditions and increased suffering. The long wait times are a result of the shortage of mental health professionals and the increasing demand for services. This delay in care can significantly impact treatment effectiveness and recovery.
-
Stigma and discrimination: The stigma surrounding mental illness prevents many from seeking help. Fear of judgment from family, friends, employers, or society at large can be a powerful deterrent, further limiting access to vital mental health services and support.
The impact of these barriers is profound. Delayed or absent treatment can lead to worsening mental health conditions, increased hospitalizations, and decreased overall quality of life. Telehealth offers a promising solution, bridging geographic gaps and increasing accessibility for those in remote areas. However, digital literacy and reliable internet access remain significant barriers for some populations.
The Shortage of Mental Health Professionals
A critical challenge facing the mental healthcare system is the significant shortage of mental health professionals, including therapists, psychiatrists, and social workers. This shortage has far-reaching consequences, exacerbating existing access issues and limiting the availability of timely and effective care.
-
Burnout and attrition: The demanding nature of the work, coupled with high caseloads and bureaucratic hurdles, leads to high rates of burnout and attrition among mental health professionals. This contributes to the overall shortage and affects the quality of care provided.
-
Lack of training and education: Insufficient training programs and limited opportunities for professional development hinder the growth and expansion of the mental health workforce. More investment in education and training is crucial to address this shortage.
-
Uneven distribution of professionals: Mental health professionals tend to concentrate in urban areas, leaving rural and underserved communities with limited access to care. Incentivizing professionals to work in underserved areas is necessary to improve equitable access.
-
Limited career opportunities: Inadequate compensation and benefits deter individuals from entering the field of mental health, further compounding the existing shortage. Addressing these limitations through improved pay and benefits packages is essential for attracting and retaining skilled professionals.
The consequences of this shortage are severe. Increased wait times, longer waitlists, and limited availability of specialized services directly impact access to care and contribute to poorer patient outcomes. Innovative strategies, such as telehealth and expanding the roles of other healthcare professionals like primary care physicians, are crucial to address this workforce gap.
Integrating Mental Healthcare into Primary Care
Integrating mental healthcare into primary care settings offers a promising strategy for improving access and improving overall healthcare. This approach involves seamlessly incorporating mental health services into routine primary care visits.
-
Early identification and intervention: Integrating mental health screenings into routine primary care visits allows for early identification of mental health concerns, enabling timely intervention and preventing conditions from worsening.
-
Collaborative care models: Establishing partnerships between primary care physicians and mental health professionals facilitates coordinated care and ensures that patients receive comprehensive treatment. This collaborative approach leverages the strengths of both disciplines to provide better patient outcomes.
-
Improved access and convenience: Making mental health services more readily available in familiar primary care settings improves access and convenience for patients. This model reduces barriers to care and makes mental health services more accessible.
-
Reduced stigma: Normalizing mental healthcare within the context of primary care helps reduce stigma and encourages patients to seek help without fear of judgment. This integration promotes open discussion and acceptance of mental health concerns.
Integrated care models have demonstrated significant benefits, including improved patient outcomes, reduced healthcare costs, and increased patient satisfaction. Successful programs show that this approach can effectively address many of the challenges associated with accessing mental healthcare.
Technological Advancements and Innovation in Mental Healthcare
Technology is rapidly transforming mental healthcare, offering new opportunities to improve access, enhance treatment, and reduce the burden on the system.
-
Telehealth platforms: Telehealth has emerged as a vital tool, expanding access to care, especially for individuals in remote areas or with mobility limitations. Online therapy sessions offer convenience and flexibility, overcoming geographical barriers.
-
Mental health apps: Numerous apps provide self-help tools, resources, and support for individuals managing their mental health. These apps offer accessible and convenient options for managing symptoms and seeking support.
-
AI-powered tools: Artificial intelligence (AI) is being employed to assist with diagnosis, treatment planning, and personalized interventions. These AI-powered tools have the potential to improve the efficiency and effectiveness of mental health services.
-
Data-driven insights: The collection and analysis of data from various sources can provide valuable insights into treatment effectiveness, identify areas for improvement, and guide policy decisions. Data-driven approaches lead to evidence-based practices and better outcomes.
While technology offers immense potential, challenges remain. Data privacy and security concerns need careful consideration. Ensuring equitable access to technology and addressing digital literacy gaps are essential to maximizing the benefits of technological advancements in mental healthcare.
Conclusion
The state of mental healthcare presents significant challenges, including limited access, workforce shortages, and systemic barriers. However, opportunities for improvement exist through increased investment in integrated care models, leveraging technology, and addressing the root causes of inequity. Improving mental healthcare requires a collaborative effort from policymakers, healthcare professionals, and individuals. Let's work together to advocate for better access to mental health services, support mental health professionals, and create a system that truly prioritizes the mental well-being of all. By addressing the challenges and seizing the opportunities for improvement, we can build a more equitable and effective mental healthcare system. Let's prioritize mental health and work towards better mental healthcare for everyone.

Featured Posts
-
 Enexis En Kampen In Juridisch Gevecht Aansluiting Stroomnet Betwist
May 02, 2025
Enexis En Kampen In Juridisch Gevecht Aansluiting Stroomnet Betwist
May 02, 2025 -
 Daisy May Cooper Faces 30 000 Legal Battle Over House Paint Colour
May 02, 2025
Daisy May Cooper Faces 30 000 Legal Battle Over House Paint Colour
May 02, 2025 -
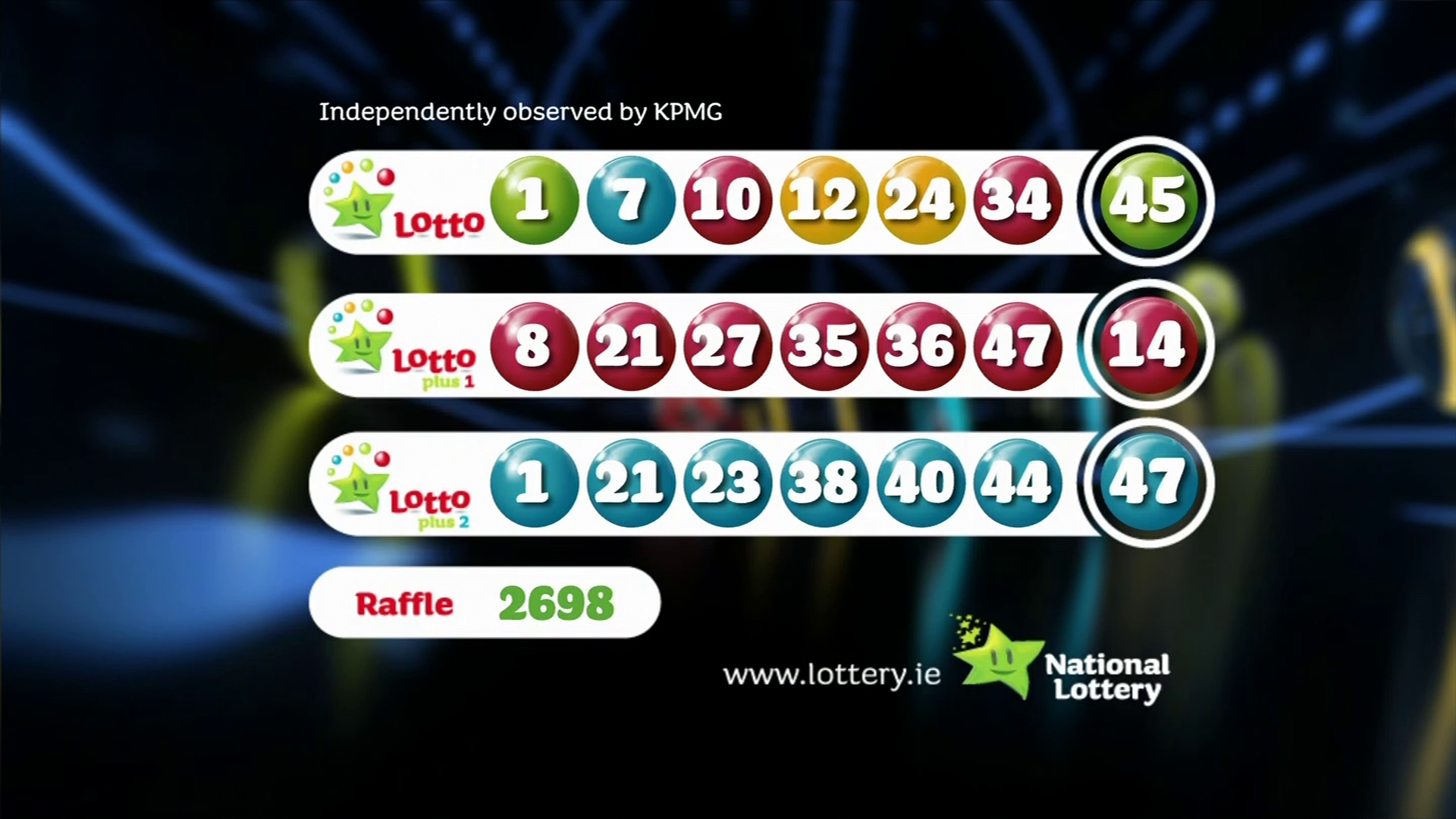 Winning Numbers Lotto Lotto Plus 1 And Lotto Plus 2 Draws
May 02, 2025
Winning Numbers Lotto Lotto Plus 1 And Lotto Plus 2 Draws
May 02, 2025 -
 Fortnite The Most Unlikely Skins To Return To The Item Shop
May 02, 2025
Fortnite The Most Unlikely Skins To Return To The Item Shop
May 02, 2025 -
 A Deep Dive Into South Koreas Housing Culture A Must See Exhibition
May 02, 2025
A Deep Dive Into South Koreas Housing Culture A Must See Exhibition
May 02, 2025
