Combating The Superbug Crisis: The Threat Of Deadly Fungi
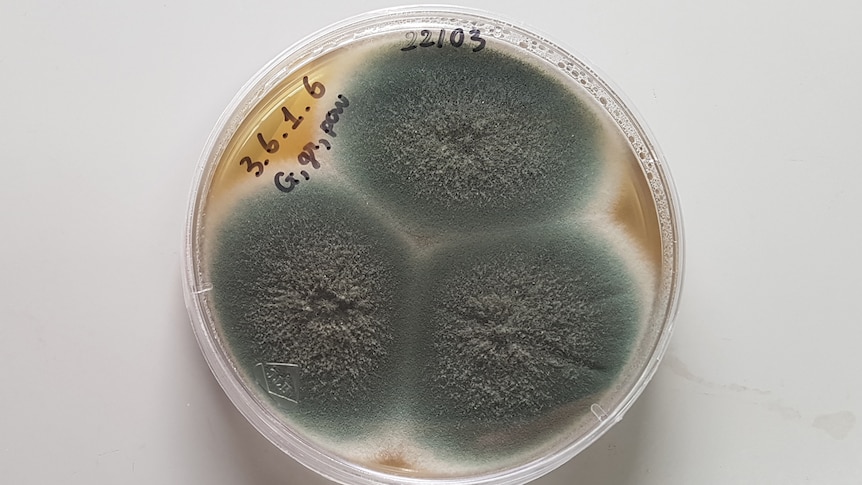
Table of Contents
The Rise of Drug-Resistant Fungi
The ability of fungi to develop resistance to antifungal drugs is a major concern. This phenomenon, driven by several factors, is transforming once-treatable infections into life-threatening conditions.
Understanding Antifungal Resistance
Antifungal resistance develops through several mechanisms:
- Overuse of antifungals: The widespread and often unnecessary use of antifungals in agriculture, human medicine, and veterinary medicine drives the selection and proliferation of resistant strains.
- Inadequate treatment regimens: Incomplete or improperly administered antifungal treatments allow resistant fungi to survive and multiply.
- Genetic mutations: Fungi, like bacteria, can undergo genetic mutations that confer resistance to antifungal drugs. These mutations can be passed on to subsequent generations, leading to the rapid spread of resistant strains.
Specific examples of increasingly resistant fungal species include Candida auris, a particularly dangerous pathogen causing bloodstream infections and often resistant to multiple antifungal drugs, and Aspergillus fumigatus, a common mold that can cause serious lung infections, especially in immunocompromised individuals. The rise of resistance in these and other deadly fungi necessitates a change in our approach to antifungal stewardship.
Contributing Factors to Resistance
Several factors contribute to the global rise of antifungal resistance:
- Increased antifungal use: The extensive use of antifungals in agriculture as pesticides and in human and veterinary medicine creates selective pressure for resistant strains to emerge.
- Lack of new antifungal drug development: The pipeline for new antifungal drugs is alarmingly thin, leaving us with limited treatment options against resistant strains. This lack of innovation in antifungal development significantly hampers our ability to tackle the growing threat of resistant deadly fungi.
- Global travel and migration: The rapid movement of people across borders facilitates the spread of resistant fungal pathogens globally.
- Immunocompromised populations: Individuals with weakened immune systems are particularly vulnerable to severe fungal infections and are more likely to develop resistant infections.
The Impact of Deadly Fungi on Global Health
The consequences of the rising prevalence of drug-resistant fungi are severe and far-reaching.
Mortality and Morbidity
Invasive fungal infections, especially those caused by resistant strains, carry high mortality rates. These infections place a substantial burden on healthcare systems globally, consuming considerable resources and increasing healthcare costs.
- Mortality rates: Estimates indicate that hundreds of thousands of deaths globally are attributable to invasive fungal infections each year. This number is expected to rise significantly unless effective countermeasures are implemented.
- Healthcare burden: Treating these infections requires extended hospital stays, intensive care, and expensive antifungal medications, leading to a substantial economic burden.
- Fungal diseases: Diseases caused by deadly fungi include candidiasis (caused by Candida species), aspergillosis (Aspergillus species), and cryptococcosis (Cryptococcus species), among others.
Vulnerable Populations
Certain populations are disproportionately affected by severe fungal infections:
- Immunocompromised individuals: People with HIV/AIDS, cancer patients undergoing chemotherapy, organ transplant recipients, and individuals with other immune deficiencies are highly susceptible to invasive fungal infections.
- Premature infants: These infants have underdeveloped immune systems, making them vulnerable to a range of fungal infections.
- Elderly individuals: Age-related decline in immune function increases susceptibility to fungal infections and makes treatment more challenging.
Combating the Threat of Deadly Fungi: Strategies and Solutions
Addressing the superbug crisis caused by deadly fungi requires a multi-pronged approach that encompasses improved diagnostics, drug development, infection prevention, and robust public health initiatives.
Improved Diagnostics
Rapid and accurate diagnosis is crucial for effective treatment of fungal infections. Improvements are needed in:
- Advanced diagnostic tools: Developing more sophisticated tools for rapid identification of fungal species and their resistance profiles.
- Improved laboratory techniques: Enhancing laboratory capacity for accurate and timely fungal identification and antifungal susceptibility testing.
- Point-of-care diagnostics: Developing diagnostic tests that can be performed at the point of care, allowing for quicker treatment decisions.
Development of New Antifungal Drugs
The urgent need for new antifungal drugs cannot be overstated:
- Targeting new fungal pathways: Research should focus on identifying novel targets within fungal cells that can be exploited for the development of new antifungal agents.
- Repurposing existing drugs: Investigating the potential of existing drugs for treating fungal infections can accelerate the drug development process.
- Exploring alternative therapies: Exploring alternative therapeutic approaches, such as phage therapy or immunotherapies, may offer promising solutions.
Infection Prevention and Control
Implementing robust infection prevention and control measures is critical:
- Improved hygiene practices: Strict adherence to hand hygiene protocols and environmental cleaning is essential to prevent the spread of fungal pathogens.
- Environmental control measures: Controlling humidity and temperature in healthcare settings can help prevent fungal growth.
- Appropriate use of antifungal medications: Promoting judicious use of antifungals to minimize the selection of resistant strains is paramount.
Public Health Initiatives
Strong public health initiatives are vital to effectively combating the threat:
- Global collaboration: International collaboration is crucial for sharing data, coordinating research efforts, and implementing effective control programs.
- Data sharing: Establishing robust surveillance systems to monitor the emergence and spread of resistant fungi is essential.
- Educational campaigns: Public awareness campaigns can educate healthcare professionals and the public about the risks of fungal infections and the importance of prevention.
Conclusion
The growing threat of deadly fungi poses a significant challenge to global health. The rise of antifungal resistance, coupled with the lack of new drugs and the vulnerability of certain populations, necessitates urgent action. By prioritizing improved diagnostics, accelerating the development of new antifungal agents, strengthening infection prevention and control measures, and fostering robust public health initiatives, we can make significant strides in fighting deadly fungi. We must work together – researchers, clinicians, policymakers, and the public – to tackle the deadly fungi threat and protect vulnerable populations from these life-threatening infections. The urgent need to address deadly fungi demands our immediate attention and sustained commitment.
Featured Posts
-
 Analysis Grand Theft Auto Vis Second Trailer And Its Bonnie And Clyde Pair
May 08, 2025
Analysis Grand Theft Auto Vis Second Trailer And Its Bonnie And Clyde Pair
May 08, 2025 -
 Xrp Etfs Potential For 800 Million In Week 1 Inflows Upon Approval
May 08, 2025
Xrp Etfs Potential For 800 Million In Week 1 Inflows Upon Approval
May 08, 2025 -
 Pakstan Ke Ezym Spahy Aym Aym Ealm Ky 12 Wyn Brsy Ke Prwgram
May 08, 2025
Pakstan Ke Ezym Spahy Aym Aym Ealm Ky 12 Wyn Brsy Ke Prwgram
May 08, 2025 -
 Golazo De Arrascaeta Flamengo Golea Y Se Corona En La Taca Guanabara
May 08, 2025
Golazo De Arrascaeta Flamengo Golea Y Se Corona En La Taca Guanabara
May 08, 2025 -
 Dc Comics Krypto The Last Dog Of Krypton A Comprehensive Review
May 08, 2025
Dc Comics Krypto The Last Dog Of Krypton A Comprehensive Review
May 08, 2025
