COVID-19 Cases Surge In Hong Kong And Singapore: Assessing India's Risk
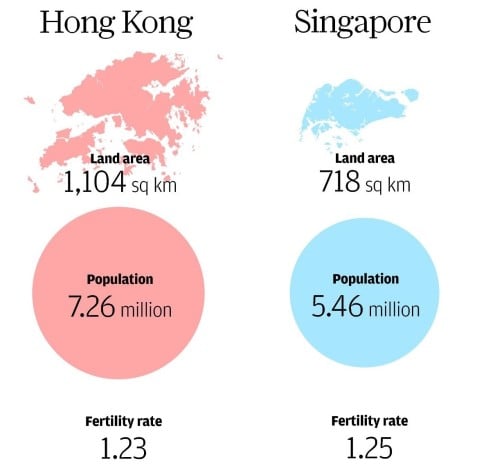
Table of Contents
Comparing Epidemiological Factors: Hong Kong, Singapore, and India
To assess India's risk, it's crucial to compare epidemiological factors across Hong Kong, Singapore, and India. These three regions, while geographically distinct, share similarities in population density and urbanization, offering a valuable comparative framework for our "India COVID surge" analysis.
Population Density and Urbanization
All three regions exhibit high population densities, particularly in urban centers. This contributes significantly to virus transmission. Hong Kong and Singapore, known for their high levels of urbanization, have seen rapid spread during previous waves. India, while having vast rural areas, also boasts mega-cities with extremely high population densities, creating hotspots for COVID-19 spread.
- Hong Kong: Extremely high population density in densely packed urban areas.
- Singapore: High population density, particularly in high-rise apartments and public housing.
- India: Extremely high population density in major cities like Mumbai, Delhi, and Kolkata; significant rural populations but rapid urbanization continues to drive population density in urban centers.
The interconnectedness facilitated by urbanization further accelerates "COVID-19 spread," making containment challenging in all three regions.
Healthcare Infrastructure
Significant differences exist in healthcare infrastructure across the three regions. Hong Kong and Singapore boast well-developed healthcare systems with high hospital bed capacity and readily available ICU beds. India, while making strides, still faces challenges in providing adequate healthcare access to its vast population. The disparity in "medical resources" is a key factor in assessing the potential impact of a surge.
- Hong Kong: Advanced healthcare infrastructure with high hospital bed capacity per capita and readily available ICU resources.
- Singapore: Excellent healthcare system with advanced medical technology and highly trained medical professionals, providing robust ICU and hospital bed capacity.
- India: A complex healthcare system with significant disparities across regions. While urban areas have better access to medical facilities, rural areas face shortages of hospital beds, ICU capacity, and trained medical personnel. Improving "India healthcare" infrastructure is crucial.
The availability of "medical resources," including ventilators and essential medications, is also a key differentiator.
Vaccination Rates and Booster Coverage
Vaccination rates and booster coverage play a critical role in determining the severity of any future outbreak. Hong Kong and Singapore have achieved high vaccination rates, although booster uptake varies. India's vaccination campaign has been extensive, but achieving widespread booster coverage remains a challenge. The effectiveness of "COVID-19 vaccines" in preventing severe illness also differs based on the vaccine type and the circulating variants. Understanding the impact of "vaccine effectiveness" on "India vaccination" progress is critical.
- Hong Kong: High vaccination rates, with varying booster uptake among different age groups.
- Singapore: High vaccination rates and significant booster coverage.
- India: Extensive vaccination campaign, but booster coverage lags behind compared to Hong Kong and Singapore.
Analyzing India's Specific Vulnerabilities
Beyond the broader comparisons, understanding India's unique vulnerabilities is crucial for assessing its "India COVID surge" risk.
Variant Prevalence and Mutation Risk
The prevalence of various COVID-19 variants and the potential for new mutations are significant concerns. India has seen several new variants emerge, underscoring the importance of "variant surveillance" and genomic sequencing. Any new, highly transmissible variant could easily overwhelm the healthcare system. Monitoring "India COVID variants" is essential.
Seasonal Factors and Climate
India's monsoon season and varying climatic conditions can influence COVID-19 transmission. Increased humidity and rainfall could affect virus spread, potentially creating seasonal peaks in transmission. Understanding the interaction between "climate change," "seasonal transmission," and "COVID-19 transmission" is critical for preparedness.
Economic and Social Factors
Poverty, overcrowding, and limited access to sanitation contribute significantly to the spread of infectious diseases in India. These "socioeconomic factors" create a vulnerable population more susceptible to severe illness and increased transmission. Addressing these factors is crucial for effective pandemic management.
Mitigation Strategies and Preparedness in India
Assessing India's preparedness requires examining its mitigation strategies and capacity to respond to a potential surge.
Government Response and Public Health Measures
The Indian government's response to the pandemic has included lockdowns, mask mandates, and vaccination campaigns. The effectiveness of these "public health measures" and "COVID-19 response India" in preventing large-scale outbreaks needs ongoing evaluation and adaptation. Strengthening "pandemic preparedness" is vital.
Testing and Contact Tracing Capabilities
India's capacity for widespread testing and effective contact tracing is crucial for containing outbreaks. Improving "COVID-19 testing India" capacity and optimizing "contact tracing" are essential.
International Collaboration and Aid
International collaboration and "pandemic aid" play a vital role in supporting India's pandemic response. Access to vaccines, medical supplies, and technical expertise are crucial for effective management of any potential surge.
Conclusion: The Risk of a COVID-19 Surge in India – Taking Action
Comparing Hong Kong, Singapore, and India reveals significant differences in healthcare infrastructure and socioeconomic factors. While India has made progress in vaccination, challenges remain in achieving widespread booster coverage, addressing socioeconomic vulnerabilities, and strengthening healthcare infrastructure. The risk of a significant "COVID-19 surge in India" remains a real possibility. Continued monitoring of "India COVID variants," proactive public health measures, and strengthened healthcare capacity are essential for minimizing the risk. Robust "COVID-19 preparedness," including improved "testing capacity" and effective "contact tracing," is paramount. We must actively work towards "preventing COVID-19 surge in India" through collaborative efforts and strategic investments in public health. This requires a concerted effort from the government, healthcare professionals, and individuals to mitigate "COVID-19 risk" in India. Stay informed, and let's work together to protect our communities.
Featured Posts
-
 Elon Musks Push To Block Open Ais Uae Deal Report Details White House Inaction
May 31, 2025
Elon Musks Push To Block Open Ais Uae Deal Report Details White House Inaction
May 31, 2025 -
 April Rainfall Is This Month Wetter Than Usual
May 31, 2025
April Rainfall Is This Month Wetter Than Usual
May 31, 2025 -
 Chinas Military Buildup Is Americas Military Industrial Complex Losing Its Edge
May 31, 2025
Chinas Military Buildup Is Americas Military Industrial Complex Losing Its Edge
May 31, 2025 -
 Samsung Tablet Vs Apple I Pad 101 Price War
May 31, 2025
Samsung Tablet Vs Apple I Pad 101 Price War
May 31, 2025 -
 Miley Cyrus Ja Bruno Mars Plagiointisyytteet Edelleen Voimassa
May 31, 2025
Miley Cyrus Ja Bruno Mars Plagiointisyytteet Edelleen Voimassa
May 31, 2025
